Solution, continued
Here are the steps they took to do this:
Rethink the all too common automatic response of providing education, a mandatory module, or competency training as the solution to performance issues.
Re‐evaluate whether education is really the best answer to the issue. Is it really the case that there is a knowledge deficit or learning gap that has caused the problem? Will a mandatory competency module fix this? This group owned the problem of too many falls and decided, based on their past use of online education modules on fall reduction with no significant reduction in fall numbers, that it was time to get creative!
Target the right action to reach the goal and harness the creative energy of the team to design and carry out the plan. This would create a targeted competency approach to truly affect the outcome.
Respond with the most fitting intervention possible one that addresses the problem in the most direct way possible and is also a good fit for the team. The team determined that the answer to how to reduce falls could be found through an exploration of the interaction of nurses, other clinicians, technicians, and patients in hospital rooms, rather than through interacting with scenarios and test questions on a computer screen. So they set up a physical space in which to explore the falls issue. They set up a room where people could play out mock scenarios in a patient room set aside for this purpose. As staff members came into the room, they were asked the outside-of-the-box question, “If you wanted your patient to fall, what would you do in this room?” Staff members messed up the room, leaving things where they don’t belong, etc. When they were done “setting the patient up to fall,” they were asked, “Do you do any of these things in your daily work routine?” The most typical answer was, “I don’t do all of them, but I do some of them. OMG!”
Outcomes
Looking at the problem differently opened the door for new insights about contributions to falls:
- “I was hurried.”
- “I was multi-tasking.”
- “I was not being present.”
The team was able to discover, accept, and work with these insights because they had come to their own conclusions through their own process. The team’s second focus —that of changing their approach to their competency process—also added to this success. They were able to have a deeper impact on the outcome by allowing their competency process to go beyond the traditional mandatory training.
Billings Clinic is a perfect example of using The Wright Competency Model for results that work. When it was decided that they would address the issue of falls, rather than slapping on a quick fix education or competency event, they brought a discussion of this problem into their competency reflection process. The Wright Competency Model is set up to encourage ownership, empowerment, and accountability to outcomes. If it is a competency issue, what type of competency assessment is needed? Is it a technical skill, critical thinking skill, or an interpersonal skill? Is it about a lack of skill in carrying out the procedure or is it that people don’t know how to speak up when the procedure is going wrong or that the culture of the organization makes speaking up unsafe?
This unit took ahold of this problem, examined it from multiple sides to really understand the issues, and took a team approach to applying a solution.
They uncovered that this was not just a simple knowledge deficit but that factors like disruptive and distractive environments and the lack of real room application in their prior educational efforts, may be contributing to falls. They chose a very creative and appropriate modality for validation and improvement which focused on critical thinking and problem solving right in their patient rooms. They used mock scenarios, group discussion, and several process frameworks. They made it fun and engaging. The staff created the process, owned it, and carried it out. Because they owned the process from beginning to end, they take greater pride in their work, and they feel good about preventing falls.
Ownership, empowerment, and accountability are keys to competency success and outcomes. Other people cannot own the work or give a competency to use and then expect the results to be stellar. That comes from the passion and engagement of a group or team. When this energy organically grows in a team, amazing things happen. The Billings Clinic team is a shining example of how out-of-the-box thinking can generate extraordinary results.
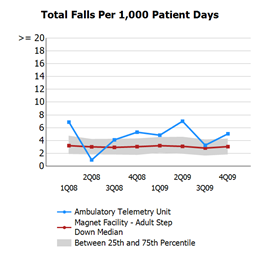
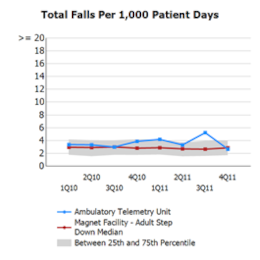
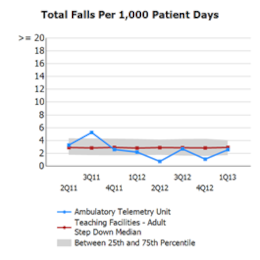
In the five years preceding this team project, Billings Clinic was below the NDNQI national average for patient falls for only two quarters, and since the 2012 implementation, they have experienced seven quarters below the national average. The research estimates a cost per hospitalization for patient falls of $33,894, and the number of preventable injuries in the United States for fiscal year 2007 of 193,566 falls. The estimated cost per fall is at a range of $1,019 to $4,235 per case, with a rate of 3.73 falls per 1,000 patient-days. By reducing falls by 68%, the Billings Clinic team not only created a safer environment for patients; they also directly impacted the bottom line of their organization!
Since realizing and sustaining these outstanding outcomes, staff members continue to identify and remove barriers, and Billings Clinic is rolling out the Wright Competency Model house-wide to use in other areas for improvement
References: